|
The growing disparity between community need for psychiatric beds and limited resources forces behavioral health patients to turn to emergency departments (EDs) as a solution. These acute settings, however, are ill-equipped for specialized behavioral health needs, leading to ED operational strain through overwhelming admissions, bed shortages and ineffective treatment. Read the infographic to discover four ways behavioral health program integration in the post-acute setting can benefit your ED and improve hospital operations and outcomes. |
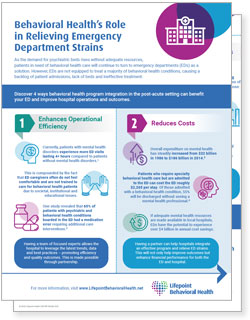
- Enhances Operational Efficiency
One in eight ED visits relates to a behavioral health condition, contributing to overcrowding and lengthy patient wait times (exceeding 12 hours at times) that compromise patient quality of care.1
This is compounded by the fact that ED caregivers often do not feel comfortable and are not trained to care for behavioral health patients due to societal, institutional, and educational issues.
One study revealed that 65% of patients with psychiatric and behavioral health complaints boarded in the ED had a medication error requiring additional care interventions.2
Having a team of focused experts allows the hospital to leverage the latest trends, data and best practices – promoting efficiency and quality outcomes. This is made possible through partnership.
- Reduces Costs
Mental health expenditure in the US has significantly increased, reaching $4.9 trillion in 2023. This rise can be attributed to rising resource and labor costs, and greater demand for comprehensive care.3
Patients who require specialty behavioral health care and are admitted to the ED can cost the ED roughly $2,265 per stay. Of those admitted with a behavioral health condition, 55% will be discharged without see a mental health professional.4
If adequate mental health resources are made available in local hospitals, EDs have the potential to experience over $4 billion in annual cost savings.4
Having a partner can help hospitals integrate an effective program and relieve ED strains. This will not only improve outcomes but enhance financial performance for both the ED and hospital.
- Lowers Length of Stay (LOS)
Behavioral health admissions in the ED have been found to occupy 42% more time than those in need of other ED-related treatment.5
These longer stays can result in more negative patient outcomes, including:• Increased suicidal ideation.
• Higher post-traumatic stress.
• Decreased productivity.
• Worsening finances.
Partnership can help hospitals gain access to a skilled interdisciplinary team specially trained in behavioral health interventions – resulting in improved patient care, outcomes, satisfaction and LOS.
- Improves Care Access
EDs have historically been the first point of entry for those experiencing behavioral health illnesses regardless of the ED’s ability to successfully diagnose and treat their condition.
Research demonstrates hospitals that incorporate behavioral health services into the post-acute setting are more likely to generate positive outcomes for patients experiencing both behavioral and physical conditions.7
Creating greater access also helps reduce the stigma around behavioral health illness and treatment while increasing education and awareness around mental health conditions.
Partnership with a trusted behavioral health provider can help a hospital achieve this accessibility and therefore help contribute to the health and well-being of their local community.
Contact us to learn how partnership with Lifepoint Behavioral Health can help your hospital address the growing mental health need in your local community and relieve ED strains.
References:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11911218/#:~:text=One%20in%20eight%20emergency%20department,alternative%20to%20the%20emergency%20department
- https://www.acep.org/globalassets/new-pdfs/information-andresource-papers/the-impact-of-psychiatric-boarders-on-theemergency-department.pdf
- https://www.globenewswire.com/newsrelease/2025/02/04/3020599/0/en/Global-Mental-Health-Market-to-Hit-Valuation-of-US-625-07-Billion-By-2033-Astute-Analytica.html
- https://www.beckershospitalreview.com/strategy/behavioral-health-simpact-on-the-emergency-department.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6754202/
- https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01616-6
- https://www.aha.org/system/files/media/file/2019/06/Market_Insights-Behavioral_Health_Report.pdf